Urethral Stricture Treatment in Turkey

What is Urethral Stricture?
Urethral stricture is the narrowing of the urethra, the urinary canal that allows urine to flow from the bladder to outside the body. This narrowing usually occurs due to scar tissue formation in the urethral wall.
Urethral stricture can cause difficulty in urine flow or completely block it. This condition may present with symptoms such as frequent urination, difficulty urinating, weak urine stream, feeling of incomplete bladder emptying, or recurrent urinary tract infections.
It often develops due to infections, trauma, surgical procedures, or prolonged use of urinary catheters. Treatment options include medication, dilation (widening) of the narrowed segment, endoscopic interventions, or surgical methods. The choice of treatment depends on the location and length of the stricture, as well as the patient’s overall health condition.
About 10% of urethral strictures are caused by lichen sclerosus. When it appears on the glans penis, it is called BXO (balanitis xerotica obliterans),and most patients with urethral strictures have this condition. In a series of 1,151 cases who underwent urethroplasty, lichen sclerosus was found as the cause in 7% of cases. Lichen sclerosus is more commonly seen in patients with hypertension, hyperlipidemia, diabetes, smokers, and obese individuals. The average age is reported as 46 ± 16 years, and the strictures tend to be much longer (pan-urethral stricture).
What Are the Causes of Urethral Stricture?
- Infection (e.g., Neisseria gonorrhoeae)
- Iatrogenic (e.g., TUR, hypospadias surgery, etc.)
- Idiopathic
- Post-traumatic (blunt or sharp injury)
- LS-BXO (lichen sclerosus – balanitis xerotica obliterans)
What Are the Symptoms of Urethral Stricture?
Urethral stricture is a serious urological condition caused by narrowing of the urinary tract, which can significantly affect urine flow. The disease typically presents with the following symptoms:
- Weak or interrupted urine stream
- Difficulty or pain during urination (dysuria)
- Feeling of incomplete bladder emptying after urination
- Blood in the urine (hematuria)
- Frequent urge to urinate
- Increased urinary tract infections
- Changes in urine direction or spraying
- Incontinence (urine leakage) or difficulty starting urination
These symptoms may vary depending on the severity of the condition and often develop gradually, which can delay diagnosis.
What Symptoms Are Seen in People with Urethral Stricture?
About 22% of patients with urethral stricture experience lower urinary tract symptoms such as difficulty urinating, weak urine flow, frequent urination, and feeling of incomplete bladder emptying. Genitourinary pain involving the genital, perineal, and suprapubic areas is seen in approximately 22.9% of patients.
Urethral stricture is not just a quality-of-life issue. In 8% of patients, the stricture causes life-threatening conditions.
Complications in patients with urethral stricture can include abscess or necrotizing infections, acute renal failure, and, very rarely, advanced-stage urethral cancer.
Does Urethral Stricture Cause Frequent Urination?
Yes, urethral stricture often leads to frequent urination. The main reason is that the narrowed urethra prevents complete bladder emptying. As a result, the bladder quickly feels full again, causing the individual to urinate frequently, often without a feeling of full emptying. This is especially noticeable at night (nocturia). Frequent urination can also result from overactive bladder muscles and may seriously affect quality of life over time.
How Is Urethral Stricture Diagnosed?
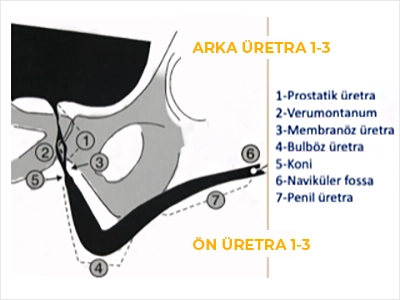
A detailed medical history is very important. If decreased urine flow is suspected, uroflowmetry can measure urine flow rates. Definitive diagnosis is made by retrograde urethrography. MR urethrography has become popular recently but provides more information about posterior urethral strictures rather than anterior ones. Cystoscopy is rarely used for diagnosis and is mainly performed when a therapeutic procedure is planned.
How Is Urethral Stricture Treated?
Urethral stricture does not resolve spontaneously and requires medical intervention. Treatment depends on the severity, duration, and cause of the stricture. For mild strictures, the first step is usually dilation—widening the urethra using special dilators. However, this method is not a permanent solution and carries a high risk of recurrence.
More effective and lasting treatments include endoscopic urethrotomy or open surgical procedures. In rare cases, especially with severe and long strictures, temporary solutions such as diverting urine directly from the bladder to the abdominal wall may be considered, but these are usually last-resort options.
Urethral Stricture Surgery
Surgery is generally one of the main treatment methods providing a permanent solution for urethral strictures. The surgical technique used varies depending on the location and length of the stricture, as well as previous treatment attempts. One of the most commonly performed techniques is internal urethrotomy (endoscopic incision),in which an incision is made at the narrowed area to widen the urethra. This procedure is minimally invasive and is usually done on an outpatient basis.
For longer or recurrent strictures, open urethroplasty is recommended. This method involves removing the narrowed segment and either reconnecting the urethral ends or reconstructing the urethra using grafts taken from the patient's own tissue, most commonly oral mucosa. Careful postoperative monitoring and management play a significant role in reducing the risk of recurrence.
Who Should Undergo Open Surgery for Urethral Stricture?
Open surgery is indicated in cases such as LS-BXO unresponsive to medical treatment, complete urethral strictures following trauma, long strictures (>1.5 cm),recurrent short bulbar strictures, strictures following hypospadias surgery, urethral injury associated with penile fracture, and sharp penetrating injuries.
What Are the Treatment Options in Open Urethral Stricture Surgery?
Open surgeries are particularly preferred for anterior urethral strictures. Endoscopic procedures may be performed for bulbar urethral strictures if they do not exceed two strictures, though these tend to recur depending on severity.
For penile urethral strictures, skin flaps from adjacent penile skin (fasciocutaneous flaps) or free grafts are used for reconstruction. The most common graft sources are mucosa taken from the inside of the cheek or lips. Occasionally, sublingual mucosa is also used. Depending on the length of the stricture, multiple grafts may be needed. The donor site usually heals very quickly. Various surgical techniques are named based on where the grafts are applied.
In the ASOPA technique, the graft is placed on the stricture’s ventral (bottom) surface. In the Barbagli technique, the graft is applied as a patch to the anterior and lateral urethral walls. The Palminteri technique involves grafting both the urethral bed and the anterior urethral wall.
What Is the Success Rate of Open Urethral Stricture Surgery?
There are many series and success rates reported in the literature for these methods. Multiple factors determine surgical success. The most important among these is selecting the right approach for the right patient. Patient-related factors such as stricture length, hardness (degree of fibrosis),whether it is a recurrent procedure, tissue vascularity, and presence of LS-BXO are crucial. However, success rates with grafts and flaps can range between 80% and 95% in first-time surgeries.
Success rates are generally higher when surgery is performed by an experienced surgeon specializing in urethral strictures, as fewer than 10% of urologists have formal training in open urethroplasty.
How Should Patients Who Have Undergone Urethral Stricture Surgery Be Followed Up?
Urinary flow rates do not decrease until the urethral diameter falls below 10 French (Fr) because abdominal straining can cause falsely good urine flow measurements. Early postoperative retrograde urethrography may also provide misleading information. The most reliable methods to detect stricture recurrence are flexible urethroscopy at 6 and 12 months after surgery.
During Endoscopic Treatment of Urethral Stricture, Should Laser or Cold Knife Be Used?
There is no difference in effectiveness between the two methods. However, hematuria and urinary retention are more frequently observed with laser urethrotomy, and laser urethrotomy is a more expensive procedure. Optical urethrotomy allows better tactile feedback of tissue resistance.
What Factors Affect the Success of Endoscopic Treatment?
The outcomes of internal endoscopic urethrotomy are worst in penile urethral strictures. Recurrence risk is higher for strictures longer than 1 cm. Success rates approach zero after more than two endoscopic interventions. Unfortunately, multiple endoscopic attempts are often made for posterior urethral strictures where grafting is not possible. To prevent recurrence in these patients, teaching self-catheterization with 14–16 Fr hydrophilic Nelaton catheters daily (TAK method) is commonly practiced.
Can the Success of Endoscopic Treatment Be Increased?
Postoperative excessive tissue healing (fibrosis) causes urethral stricture recurrence. Various substances have been applied into urethral tissue to reduce fibrosis and improve success rates.
These include mitomycin C, steroids (triamcinolone, prednisolone),combinations of steroid-mitomycin C-N-acetylcysteine, platelet-rich plasma, hyaluronic acid-carboxymethylcellulose, captopril, 192-Iridium brachytherapy, paclitaxel, and tamoxifen. Among these, mitomycin C is the most commonly used and has the strongest scientific support. It has anti-fibroblast and anti-collagen properties, with many studies demonstrating its efficacy in reducing stricture recurrence.
What Are the Treatment Approaches for Posterior Urethral Strictures?
Posterior urethral strictures mainly result from trauma and iatrogenic causes. Urethral bleeding in patients with pelvic trauma is an important sign suggesting injury. Catheterization should be avoided in these patients because a partial tear can become a complete rupture. Although some surgeons prefer early repair, it is important to consider that these patients often have other injuries.
Waiting for the final condition to stabilize before reconstruction is generally more appropriate. Therefore, in patients diagnosed with posterior urethral injury by retrograde urethrography, a suprapubic catheter is usually placed. After 3 to 6 months, combined voiding cystourethrography (VCUG) and sometimes MR urethrography are performed to assess urethral and pelvic fracture status.
Opening the bladder neck during combined VCUG is crucial and can be facilitated by giving the patient 20 mg tadalafil the night before. To precisely determine the stricture length, flexible cystoscopy is performed simultaneously via the urethra and suprapubic tract, which also evaluates bladder neck status.
Since strictures commonly occur at the bulbomembranous junction, they are accessed perineally, incised, and healthy urethral ends are reconnected (anastomosis). Posterior urethral anastomotic urethroplasty tends to be prone to bleeding and is a more complex surgery requiring expertise in techniques like pubectomy and crural separation. Therefore, it is advisable that experienced surgeons perform these operations.
Is the Success Rate of Posterior Urethral Anastomotic Urethroplasty Low?
Except in cases where the bladder neck is completely lost, success rates of these surgeries by experienced surgeons range between 80% and 90%.
Does Urethral Stricture Affect Sexual Function?
Yes, urethral stricture can affect sexual function in men. The most common problems include ejaculatory disorders and painful ejaculation. Increased pressure in the urethra due to stricture can make semen exit difficult or alter its direction. Additionally, increased urinary tract infections may cause pain and decreased libido.
Psychological effects should not be overlooked. Particularly in younger patients, recurrent urinary problems and anxiety about sexual performance can damage self-confidence. These sexual complications often improve after surgery, but in some cases, pelvic floor therapy or psychological support may be necessary.
Is Urethral Stricture Related to the Prostate?
Urethral stricture and prostate diseases are often confused because they share similar symptoms; however, these are completely different conditions. Prostate enlargement (BPH) occurs when the prostate gland grows with age and compresses the urinary tract, while urethral stricture refers to a narrowing directly within the structure of the urethra itself. Urethral strictures can develop due to trauma, infections, previous surgeries, or congenital reasons.
Both conditions cause similar complaints such as weak urine flow, frequent urination, and the feeling of incomplete bladder emptying. Therefore, differential diagnosis requires uroflowmetry, cystoscopy, or imaging methods.
What Should Be Done to Prevent Urethral Stricture Recurrence?
There are several preventive strategies to avoid recurrence of urethral stricture. Firstly, it is essential to provide complete and appropriate treatment targeting the cause of the stricture. After surgery, regular follow-up and, if necessary, preventive dilation protocols recommended by the doctor should be applied.
Additionally, protecting against urinary tract infections, avoiding trauma, and ensuring catheterization is performed under sterile conditions reduce the risk of recurrence. Patients should pay attention to hydration, maintain hygiene, and protect themselves against sexually transmitted infections. In the long term, maintaining a healthy lifestyle and taking early symptoms seriously play a critical role in preventing recurrence.
