Bladder Pain Syndrome Treatment Turkey

What is Bladder Pain Syndrome (BPS)?
Bladder Pain Syndrome was first described by Skene in 1887 and has since had many different definitions. In 2009, the Society of Urodynamics and Female Urology defined it as pain, pressure, and discomfort felt in the bladder, lasting longer than 6 weeks, without an identifiable cause, accompanied by lower urinary tract symptoms.

How Is Bladder Pain Syndrome Diagnosed?
First, the patient should have symptoms of bladder pain along with frequent urination. Cystoscopy findings play a crucial role in supporting the diagnosis.
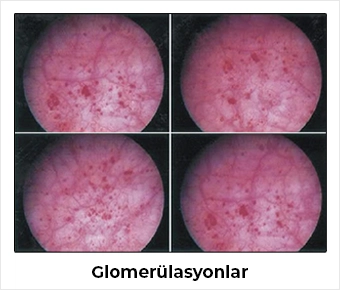
Under anesthesia, the bladder is filled and emptied twice with normal saline at a pressure of 80-100 cmH2O for 1-2 minutes each time. Afterward, cystoscopy is performed to investigate the presence of glomerulations (bleeding spots) and Hunner’s ulcers.
The glomerulations should be widespread, occurring in at least three quadrants of the bladder, with at least 10 lesions in each quadrant.
Is Bladder Biopsy Important?
There is no specific histological finding pathognomonic for bladder pain syndrome, and diagnosis cannot be made solely based on pathology without cardinal symptoms.
Normal bladder biopsies are frequently seen in symptomatic patients. However, the presence of mast cells in the biopsy can strengthen the diagnosis.
In Which Patients Is the Diagnosis of Bladder Pain Syndrome Suspicious?
The diagnosis is considered suspicious in patients who, during cystometry, have bladder capacity over 350 ml, no strong urge to urinate when the bladder contains 150 ml of fluid, presence of phasic involuntary contractions during cystometry, symptom duration shorter than 9 months, absence of nocturia, symptoms improving with antibiotics/antiseptics, anticholinergic or antispasmodic drugs, urinating fewer than eight times during the day, recent diagnosis (within last 3 months) of bacterial cystitis or prostatitis, presence of stones in the bladder or ureters, active genital herpes infection, cancers of the uterus/cervix/vagina/urethra, urethral diverticulum, cystitis due to cyclophosphamide or other chemicals, tuberculosis or radiation cystitis, or benign or malignant bladder tumors.
At What Ages Does Bladder Pain Syndrome Occur?
Previously, diagnosis before age 18 was considered suspicious, but now it is known that bladder pain syndrome can occur even in younger ages. It is mostly seen in middle-aged adults.
How Common Is Bladder Pain Syndrome in the Population?
Recent studies show an increasing prevalence of bladder pain syndrome, varying by country. On average, it occurs in about 2.5-2.7% of women. Among first-degree relatives of women with MAS/IC, the prevalence is 17 times higher than in the general population, indicating a genetic component in the disease’s development. European Urology Guidelines report a female-to-male ratio of 10:1, with the syndrome much more common in women. In men, bladder pain syndrome tends to appear at older ages and Hunner’s ulcers are detected more frequently.
Quality of Life in Patients with Bladder Pain Syndrome
Although symptoms may fluctuate, their severity generally does not worsen over time. These patients are found to miss work due to health issues six times more than the general population.
Depression, anxiety, and general mental health disorders are more common. Sexual desire and frequency of orgasm are also reduced.
What Causes Bladder Pain Syndrome?
The integrity of the bladder’s inner lining, called the urothelium, is disrupted. In these patients, levels of APF (anti-proliferative factor),HB-EGF (heparin-binding epidermal growth factor–like growth factor),and EGF (epidermal growth factor) in the urine increase. Particularly, the increase in APF inhibits the repair of the damaged urothelium.
Activation of sensory nerves, especially pain fibers, triggers the release of neuropeptides such as substance P, neurokinin A, and calcitonin gene-related peptide. These neuropeptides increase vascular permeability, leading to leukocyte adhesion and tissue edema. At the same time, mast cells degranulate and release other potent mediators, causing epithelial cell damage and increased permeability.
In patients with bladder pain syndrome, elevated urinary catecholamines have been observed. It remains unclear whether increased sympathetic activity is a cause of the syndrome or a consequence of long-term pain and pathological voiding patterns. Chronic stress is often investigated as a contributing factor.
How Is Bladder Pain Syndrome Treated?
Treatment for bladder pain syndrome varies for each patient because symptoms and severity differ individually. Generally, the first step involves lifestyle and dietary changes. Avoiding acidic, spicy, or caffeinated foods and beverages may help alleviate symptoms. Pelvic floor physical therapy to relax pelvic muscles can also be effective in reducing pain.
Medication is usually introduced to control symptoms. Antihistamines aim to reduce inflammation in the bladder wall; pain relievers and some antidepressants are used to manage pain. In some cases, direct bladder instillations (medications placed inside the bladder) may be applied. In advanced cases, nerve stimulation therapies or surgical options may be considered. The treatment process typically requires a multidisciplinary and patient approach, so regular communication between patients and their doctors is essential.
Medications Used in the Treatment of Bladder Pain Syndrome
According to literature and urology guidelines, many oral medications have been tried. Among these, two drugs have the highest level of evidence and recommendation: amitriptyline (Laroxyl) and pentosan polysulfate (Elmiron).
Are There Medications Instilled Directly Into the Bladder for the Treatment of Bladder Pain Syndrome?
For many years, various protocols have been applied for this purpose. Typically, medication cocktails are instilled into the bladder twice a week for about 3 months. The medications are held inside the bladder for approximately one hour. Most of these cocktails contain lidocaine, heparin, bicarbonate, pentosan polysulfate, and corticosteroids. Among the drugs instilled into the bladder, the one with the highest level of evidence and recommendation is DMSO (dimethyl sulfoxide). Hyaluronic acid is also frequently used for bladder instillation.
Is Botulinum (Botox) Injected into the Bladder for Bladder Pain Syndrome Treatment?
There is no FDA approval for the use of botulinum toxin in bladder pain syndrome, but many studies have demonstrated benefits of injecting 100 units into the trigone area. For patients who do not adequately respond to other treatments, botulinum toxin injections into the bladder should be considered an important treatment option.
Are There Other Treatment Options for Bladder Pain Syndrome?
For patients with bladder pain syndrome who have ulcers, endoscopic resection or cauterization of these lesions has shown positive effects in the literature. Sacral neuromodulation is an expensive method but is used in resistant cases. Good results have also been reported with pretibial nerve stimulation. The benefits of acupuncture for this purpose remain debated in the literature. In patients resistant to all treatments, bladder removal surgery may be performed.
Is There a Relationship Between Bladder Pain Syndrome and Diet?
It is known that symptoms can be triggered by many foods, but there is no universal diet program suitable for all patients. Patients should be aware of which foods and beverages trigger their symptoms and avoid them accordingly. Alcohol, acidic beverages, and cola drinks are among the most commonly blamed triggers.
